All-In-One
Secure Client
Communication platform for Families & Therapists
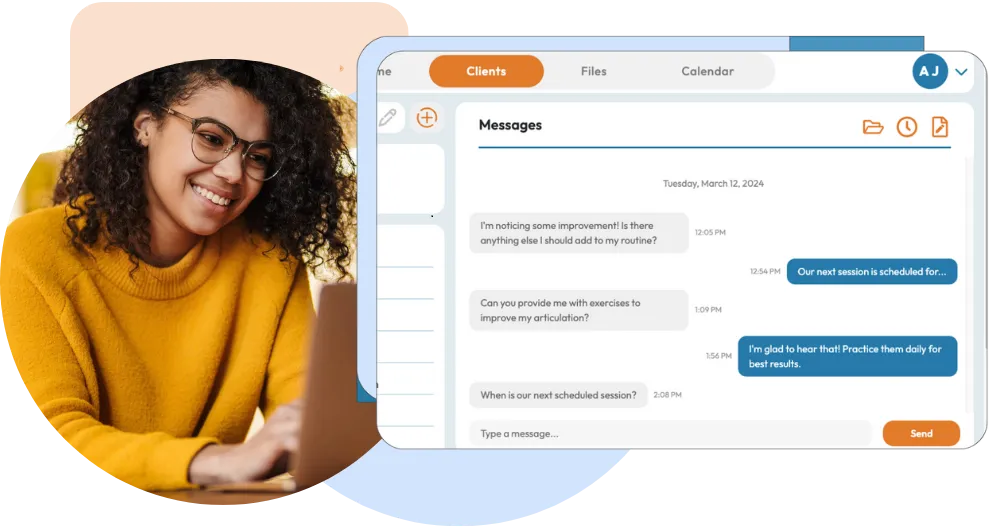
Welcome to Azelo, a HIPAA-compliant, 2-way text messaging software for healthcare providers. Easily schedule messages, capture e-signatures, and communicate in your client's preferred language using automatic translation.
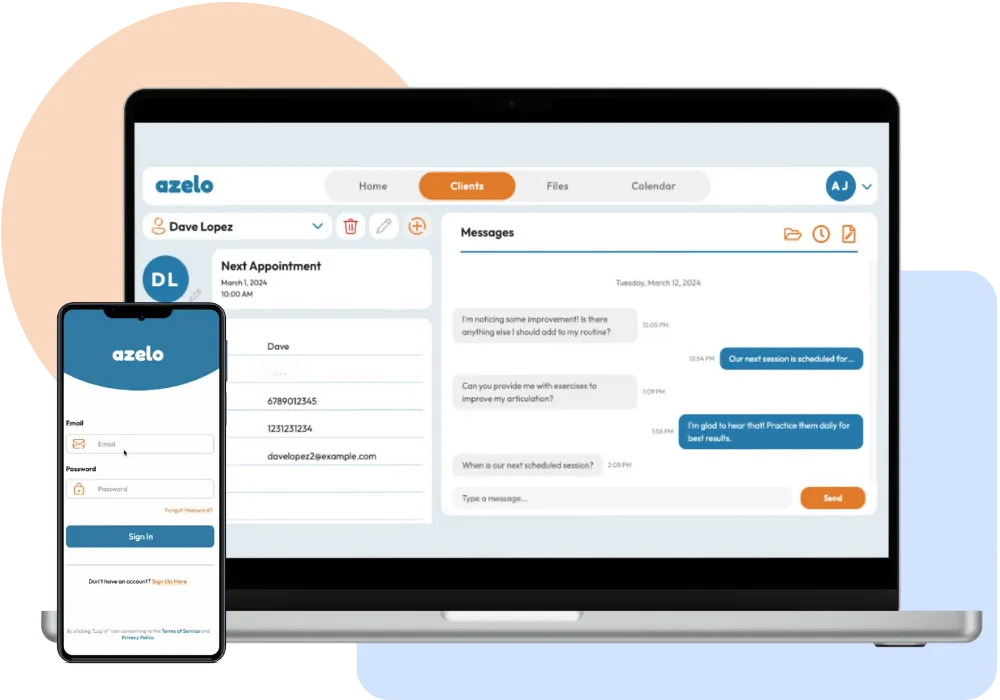
What is Azelo?
Seamless, secure communication for allied healthcare professionals.
Azelo is a secure and convenient text communication platform designed to connect you with your clients wherever they are. Our HIPAA-compliant solution revolutionizes patient care by simplifying communication through text messaging. Simplify your communication and focus on delivering great care.
Why Choose Azelo?
Built for healthcare professionals who need a simpler way to connect with clients.

Eliminate Missed Calls and Emails
Azelo’s direct and secure text messaging allows you to bypass missed calls and emails, reaching clients through HIPAA-compliant messaging instantly.
Improve Treatment Outcomes
Enhance client care with Azelo’s easy-to-use tools like automated follow-ups, secure messaging, and the ability to collect e-signatures directly through text. These features ensure clients stay on track with their treatment plans, improving overall outcomes.
Boost Client Engagement
Use Azelo’s text translation feature to communicate with clients in their preferred language, fostering more personal and effective communication.
Reduce No-Shows
With Azelo’s automated appointment reminders and customizable message scheduling, clients receive timely notifications, helping ensure they never miss an appointment.
What is Azelo?
Who is Azelo For?
Built by Therapists, for Therapists
Azelo was created by a therapist who understands the challenges of managing client communication. Azelo is designed for healthcare professionals who want to connect with their clients easily and efficiently. Our specialized platform is built to elevate client care for speech therapists, occupational therapists, social workers, mental health professionals and home health providers. Azelo is built to make connecting with your clients easily, securely and efficiently.
Resources and News
Stay informed with expert tips on enhancing client interaction, streamlining communication, and optimizing your healthcare practice.
Writing Effective SOAP Notes for Speech-Language Therapy: A Guide for Early Intervention Therapists
SOAP notes are essential for documenting therapy sessions in speech-language therapy, other medical settings, and Early Intervention (EI). These notes provide a clear, structured format to track progr... ...more
All blogs
November 14, 2025•12 min read

Using HIPAA-Compliant Texting
In the world of allied health, the role of parent coaching has become increasingly important. Speech therapists, occupational therapists, and other professionals working with children are not just foc... ...more
All blogs
November 14, 2025•8 min read

How AI is Transforming Speech Therapy
In recent years, Artificial Intelligence (AI) has made significant inroads into various fields, and speech therapy is no exception. Speech-Language Pathologists (SLPs) are increasingly leveraging AI t... ...more
All blogs
November 14, 2025•9 min read
Get Started with Azelo Today
Ready to take the next step? Choose your plan and start improving communication with your patients today. Get immediate access to Azelo's HIPAA-compliant tools, including scheduled messages, text translation, and e-signatures.

Quick Links
© 2025 Azelo. All Rights Reserved | Privacy Policy| Terms of Service | Website by Taft Systems|azelo.app privacy
